- Informera kvinnan och inhämta samtycke.
- Säkerställ adekvat bedövning innan klippet läggs, antingen inre PDB eller infiltration med t ex 5-10 ml Xylocain på planerad plats för klippet.
- Lägg klippet när huvudet kronar (vid sugklocka är då hela klockan synlig i introitus), då vävnaderna är uttänjda och mindre blodfyllda.
- Lägg klippet i början av en värk. Blödningsmängden ökar om klippet läggs för tidigt.
- Episiotomi lateralt eller mediolateralt. Klippets vinkel är viktigast och bör vara 60° från medellinjen.
- För att åstadkomma rätt vinkel, stå gärna med vänster sida mot patienten och för in vänster pek- och långfinger innanför slidöppningen mellan föregående fosterdel och slidväggen. För in den halvöppna saxen mellan pek- och långfinger och rikta den mot sittbensknölen, klockan 4 i denna position. Om du är vänsterhänt kan du stå med höger sida mot patienten och rikta saxen mot kl 8.
- Klipp 3-5 cm långt för att avlasta muskelvävnaden. Saxen bör vara vass. Sträva efter att åstadkomma klipplängden med ett (ej flera) saxtag.
- När klippet lagts måste framfödandet kontrolleras så att det inte går för fort. Fortsatt god kommunikation med kvinnan och perinealskydd är av största vikt.
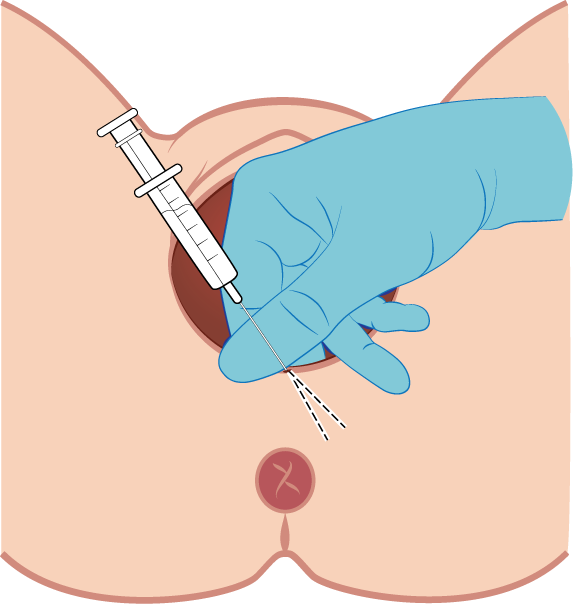
Figur Lateral infiltration inför klipp
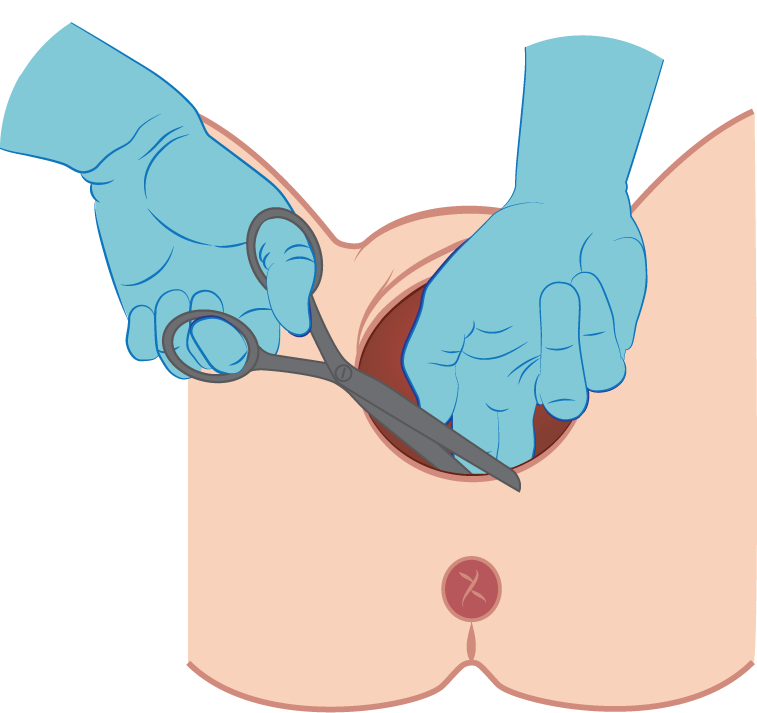
Figur Klippvinkel
Bilden ovan visar korrekt vinkel för att åstadkomma mediolateral episiotomi med 60 graders vinkel.
Komplikationer av episiotomi
Även vid episiotomi finns en risk för skada på sfinktermuskulaturen trots att klippet utförts för att skydda denna. Det finns inga belägg för att lateral episiotomi skadar levatormuskulaturen eller skyddar mot levatorskada.
Episiotomi kan vara associerat med ökad användning av analgetika och blödning postpartum, men det vetenskapliga underlaget för det är svagt. Hos förstföderskor som fött med sugklocka och lateral episiotomi eller ingen episiotomi var det ingen skillnad i blödningsmängd eller smärtskattning första dagarna på BB eller vid 2 månader, men fler kvinnor använde smärtstillande efter förlossningen i klippgruppen. Det var ingen skillnad i hur länge smärtlindring behövdes.
Lateral episiotomi kan innebära en ökad risk för sårinfektion och sårruptur.
